Metabolic syndrome (‘MS’) is a medical term that applies to various health conditions. We will get into each condition shortly. For now, just think of MS as a wide-ranging medical condition often resulting from being overweight or obese.
Nobody likes facing the potentiality of a dangerous medical condition, and MS is no different. However, we can make a conscious choice to make some lifestyle choices – and decrease the risk of developing the condition.
Causes of M.S.
Inactive lifestyles and/or a genetic predisposition are usually responsible for metabolic syndrome. Another word for inactivity is ‘sedentary,’ which most medical professionals use to describe a desk-bound, lazy way of living.
Of course, being sedentary is a risk factor for being overweight or obese; both conditions can create many other health issues.
As being overweight or obese correlates to M.S., here is a point-by-point description of what regularly happens within the body:
- A healthy digestive system will actively break down the foods you consume into sugar, or glucose. The chemical responsible for this conversion is insulin.
- Overweightness or obesity may stimulate problems within the digestive system.
- Sometimes, the overweight or obese person’s digestive system goes awry.
- s a result, their cells do not respond to insulin, causing blood sugar to spike. This condition is called insulin resistance.
“Who’s at risk?”
Statistically, certain demographics of the population are more at risk than others. Also, people with certain health conditions are more likely to develop metabolic syndrome.
- Age: Risk of MS increases as you get older.
- Race: Latin Americans “appear to be at the greatest risk of developing metabolic syndrome,” followed by Caucasians and African-Americans.
- Diabetes: Risk of MS is higher if you have a family history of type 2 diabetes.
- Obesity: Disproportionate amounts of fat around the abdomen increases the risk of MS.
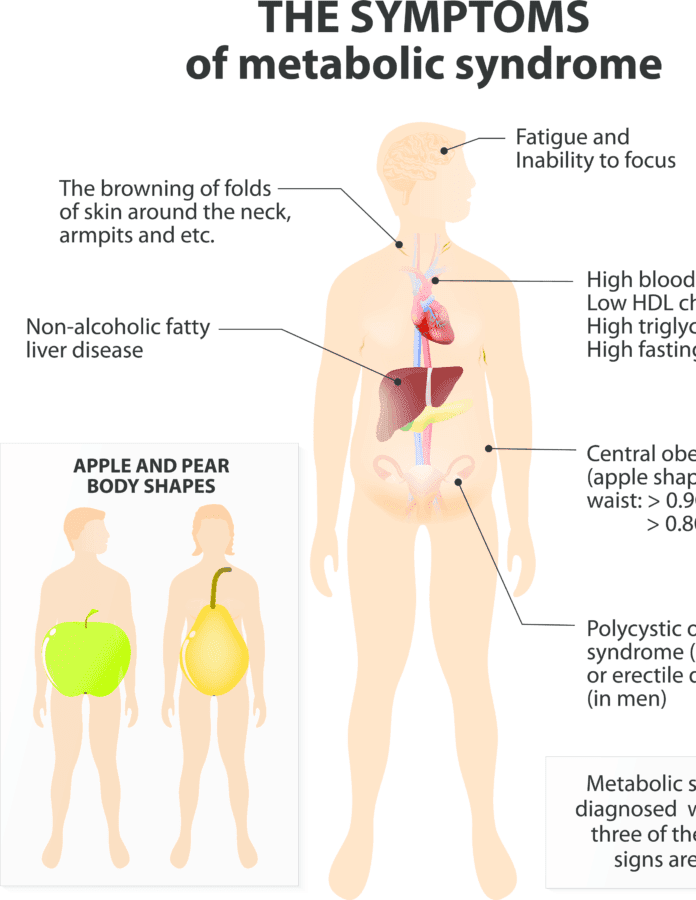
- Diseases: Cardiovascular disease, nonalcoholic fatty liver disease, and polycystic ovary syndrome increase the risk of MS.
6 Signs of Metabolic Syndrome
As we go through the six most common signs of metabolic syndrome, please bear in mind that some metabolic disorders have no symptoms; this is a critical point.
The following information is based on guidelines set forth by the National Heart, Lung, and Blood Institute (NHLBI) and the American Heart Association (AHA).
Per these criteria, any person with three or more signs meet the standards for M.S.
1. High blood pressure [Hypertension]
Healthy blood pressure is below 120 systolic or 80 diastolic (120/80). Blood pressure between 120/80 and 140/90 is considered “normal.” Any blood pressure reading above 140/90 is a sign of pre-hypertension.
Symptoms of high blood pressure: dizziness, headaches, chest pain, shortness of breath, nosebleeds.
2. High blood sugar
For a person without diabetes, a “fasting blood sugar” reading (a measure taken following a 24-hour fast) is under 100 mg per deciliter (dl).
Typically, blood sugar (or blood glucose) is considered too high if it exceeds 130 mg/dl before a meal or 180 mg/dl shortly afterward. Under most circumstances, high blood glucose symptoms do not surface until levels exceed 250 mg/dl.
Symptoms of high blood glucose: blurred vision, fatigue, headaches, increased thirst, frequent urination, trouble focusing (“brain fog”).
3. Low high-density lipoprotein (HDL) cholesterol
HDL is considered the “good” cholesterol type and is vital for heart health. Despite popular opinion, cholesterol is an essential fat and is a crucial substance for every cell.
For men, HDL level of less than 40 mg/dl is considered too low. For women, it is HDL levels below 50 mg/dl.
Smoking, poor diet, and lack of exercise are commonly cited reasons for low HDL.
4. Large waist circumference
A large waist size is usually an indication of excess belly fat. Per the Mayo Clinic, a “large waist circumference” is defined as:
– “a waistline that measures at least 35 inches (89 centimeters) for women and 40 inches (102 centimeters) for men.”
5. High triglyceride level
Triglycerides are one of three fatty acid groups and are in our blood. As we eat, the body transfers any calories not needed for energy into triglycerides and stores them in your fat cells. As the body needs energy, this lipid releases from the hormones within the pancreas.
- Normal levels: less than 150 mg/dl
- Borderline: 150-200 mg/dl
- High: greater than 200 mg/dl
- Dangerously high: > 500 mg/dl (may cause pancreatic inflammation).
6. Obesity
Obesity is defined as being excessively overweight and is the top risk factor for developing metabolic syndrome. Typically, a measure called the Body Mass Index (BMI) determines a person’s degree of obesity.
While an imperfect method, BMI may help determine whether they’re overweight or obese.
Please note that it is important to consider body type – a simple “eye test” will suffice (not medically recommended, obviously).
First, here’s how to calculate BMI in kilograms (kg) and centimeters (cm):
– Weight (kg) divided by height (cm)
Here’s how to calculate BMI in pounds (lb.) and inches (in):
– LB/IN x .45
Second, here is the BMI range (applies to men and women) for underweight, normal weight, overweight, and obese:
Underweight: BMI < 18.5
Normal: BMI 18.5-24.9
Overweight: BMI 25.0-29.9
Obese (and category):
Class 1: BMI 30 < 35
Class2: BMI 35 < 40
Class 3: BMI > 40 (“extreme” or “severe” obesity)
Decrease your risk of M.S.
Here are a few ways to lower your risk of metabolic syndrome:
- Lose weight: Even a 10% reduction helps significantly.
- Exercise: Aim for 30-45 minutes of moderate physical activity per day.
- Know your family history of risk-related diseases (see above), and make the appropriate changes.
- Eat a well-balanced and nutritious diet: Prioritize fruits, vegetables, whole grains, and lean meats.
- Do not fast without consulting a medical professional.