Documentation of humans engaging in pregnancy-prevention techniques such as abstinence and withdrawal dates back to before 3000 B.C. When these birth control methods ceased to be reliable, those early people turned to condoms and spermicides made out of everything from fish bladders to linen cloth. (1.)
It wasn’t until 1960 that a woman named Margaret Sanger introduced the first oral contraceptive, called Envoid. In her mid-80s, she raised $150,000 for the research project and product development process.
Originally, the US Supreme Court approved oral contraceptives only for use by married women not looking to conceive. Regulations denied access to other women until new legislation overturned the law nearly a decade later.
THE INTRODUCTION OF IUDs
Intrauterine devices, or IUDs, came about in 1968 as an alternative to daily medication. In 1974, they were slowly removed from the U.S. market after a slew of lawsuits against one particular brand: the Dalkon Shield IUD.
The 1980s and 90s saw rapid expansion in the types of birth control available. Introduced were drugs with low-dose hormones, the popular ParaGard IUD, contraceptive implants and injectables, female condoms, and the Plan B pill.
A new century dawned, and it brought forth even more contraceptive advancement in terms of availability, safety, and options. New treatment options such as the hormonal patch, vaginal ring, and female sterilization offered females even more methods to choose from.
Today, birth control is widely available in America. But it remains a highly controversial and political topic. While undoubtedly effective at preventing pregnancy, each type of contraceptive also comes with many risks that doctors often don’t disclose to women.
RISKS AND ALLEGED BENEFITS OF DIFFERENT CONTRACEPTIVE METHODS
Oral contraceptives
Birth control pills include any combination of synthetic female reproductive hormones taken orally. There are over 30 different types available in the United States, most of which include 21 hormonally active pills and seven which contain no hormones.
-
- Pros
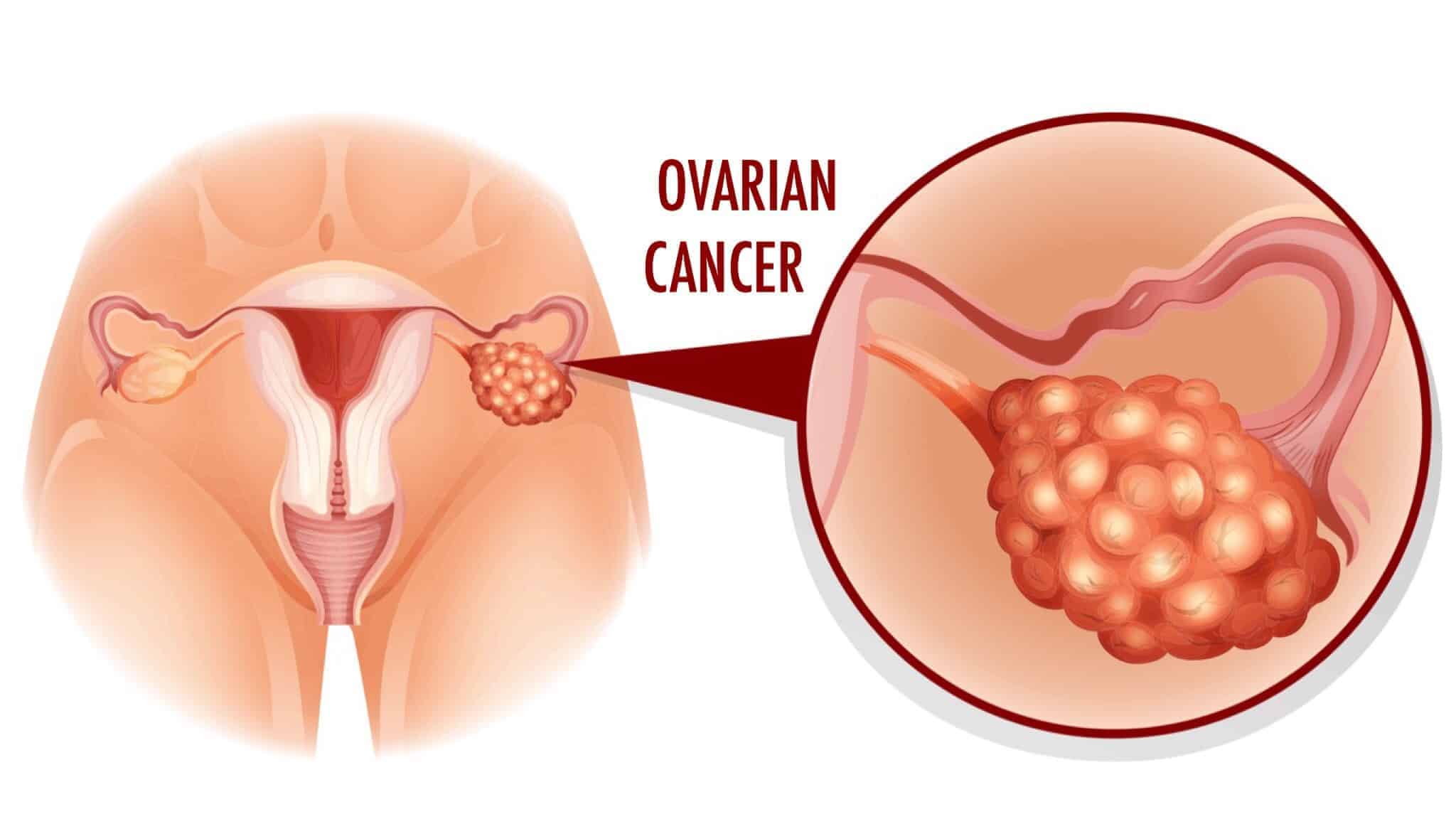
- Prevention of certain diseases such as benign breast disease, pelvic inflammatory disease, functional cysts, ectopic pregnancies, and certain ovarian and endometrial cancers.
- Women with a history of irregular menstrual periods can expect a bleed on the same week each month while taking the non-active pills.
- An effectiveness rate of between .1 and 5% depending on the accuracy of use.
- Pros
- Cons
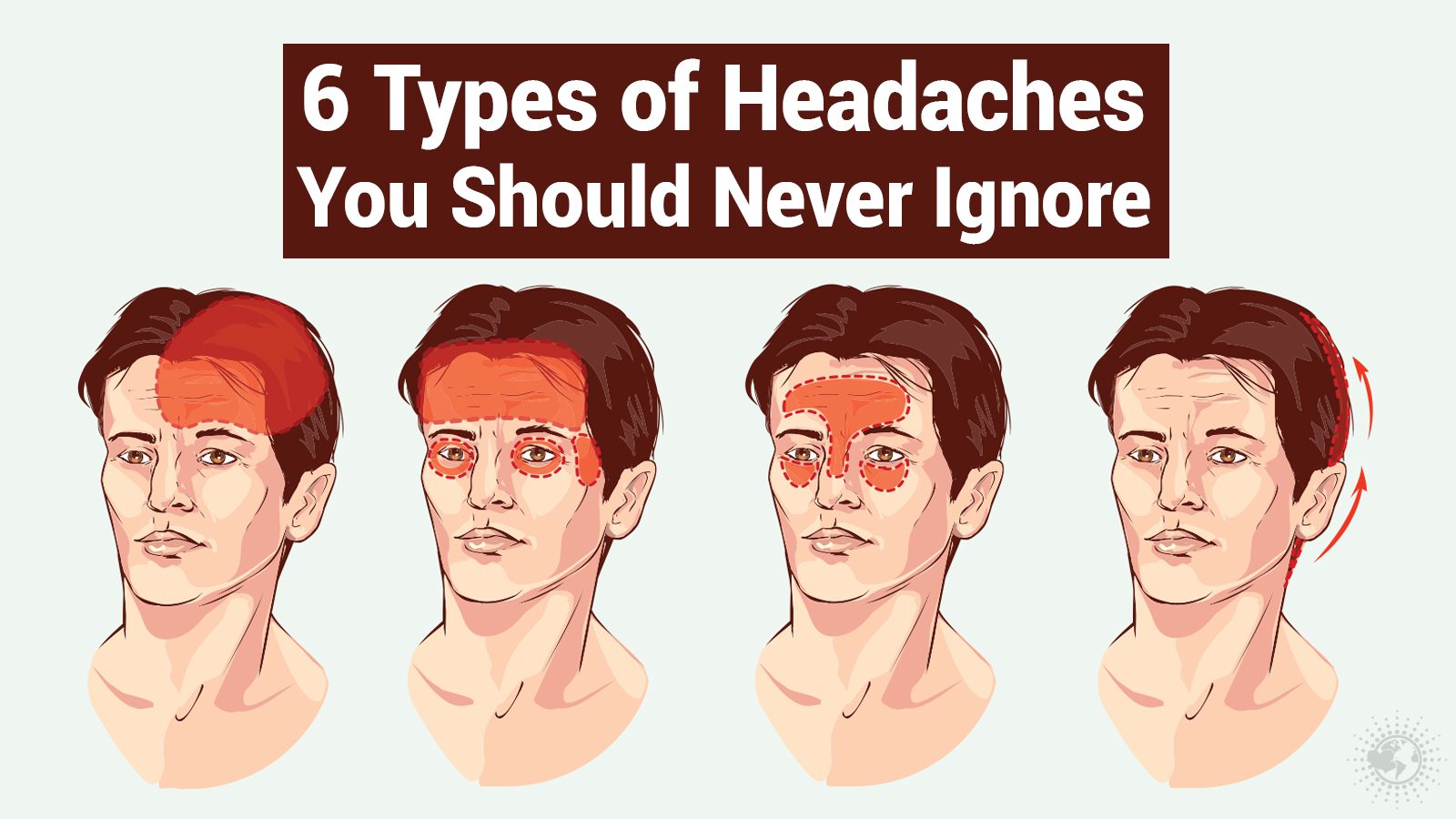
- Physical symptoms such as nausea, weight gain, breast tenderness, breakthrough bleeding, absent periods, headaches, depression, anxiety, and diminished libido.
- Increased risk of blood clots, especially among women who are over the age of 35, have elevated cholesterol levels, diabetes, high blood pressure, or are obese.
- There is also a loose correlation between oral contraception and breast and cervical cancers.
Contraceptive implant
Known as Nexplanon, the contraceptive implant is placed in the upper arm and releases a slow, steady dose of progestin (the synthetic form of progesterone, a naturally-occurring female reproductive hormone.) It is generally very effective for up to three years. (2.)
- Pros
- Comparable to surgical sterilization in terms of effectiveness. Pregnancy rates increase from about .2% to .5% over three years.
- Women typically regain fertility shortly after removal.
- Cons
- Physical symptoms include menstrual changes, weight gain, headaches, altered mood, growth of facial hair, and acne.
Birth control patch
Under the brand name Ortho Evra, the transdermal patch releases estrogen and progesterone directly into the skin. It contains a one-week supply of hormones equivalent to the lowest daily dose of oral contraception.
- Pros
- Failure rate of only one out of every 100 women.
- Women don’t have to remember to take a pill each day. Instead, they apply a new patch every week for three weeks and remove it on week four when they expect a menstrual cycle.
- Cons
- Similar to those experienced by women taking oral contraceptives, in addition to skin irritation where the patch is placed.
- The patch may come off and go unnoticed.
Vaginal ring
Vaginal rings deliver a combination of estrogen and progesterone, released slowly and absorbed through the vaginal walls.
- Pros
- Fewer symptomatic side effects than oral contraceptives, implants, and patches with similar effectiveness.
- Like the patch, vaginal rings are left in for three weeks and removed for one, during which time menses are expected.
- Cons
- If the vaginal ring happens to fall out for more than three hours, a backup form of contraception must be readily available in order to prevent pregnancy.
Injection
Depo-Provera, or an injectable synthetic hormone, stops ovulation for up to three months by preventing the ovaries from releasing eggs.
- Pros
- The shot doesn’t interact negatively with other medications and its effectiveness isn’t decreased in heavier patients.
- Failure rate of just .3% during the first year.
- Doesn’t produce the serious adverse side effects seen with estrogen, such as blood clotting.
- Lowers the risk for certain types of endometrial cancers.
- Cons
- A delayed return to fertility after coming off the injection.
- Possible bone-density loss.
- Weight gain, depression, and menstrual irregularities that can persist for up to one year following the last injection.
Intrauterine devices (IUDs)
IUDs are small, T-shaped plastic devices placed inside the uterus. Two types of IUDs are available: hormonal and copper.
- Pros
- One of the most effective types of birth control available. Only eight out of every 1,000 women with an IUD will become pregnant within the first year of use.
- Constant protection with no need to remember anything.
- Low risk of side effects compared to other birth control methods.
- Longevity. IUDs can remain in place for up to ten years, and as such, are relatively inexpensive over time.
- Cons
- Can only be inserted and removed by a trained professional.
- Can be spontaneously expelled, a phenomenon that most commonly occurs during menstruation.
- May perforate the uterine wall when inserted (this only occurs in 1-3 per 1,000 cases.)
It is worth noting the Fertility Awareness Method is a free, non-hormonal alternative to contraception. This involves a woman tracking her basal body temperature and cervical mucus to determine when she is fertile. There are no risks to this method aside from unintended pregnancy.
THE TOP 6 MYTHS ABOUT BIRTH CONTROL YOUR DOCTOR MAY HAVE TOLD YOU
1: It regulates hormones and menstrual cycles
This is likely the most common myth regarding birth control. Here’s what happens. Women go to their doctors complaining about irregular menses, painful periods, acne, or a number of other symptoms associated with menstruation. The doctor writes a prescription for the pill. While it may induce a monthly bleed and reduce unwanted symptoms, birth control is by no means a solution. In fact, it doesn’t address the underlying issue. (3.)
2: It heals endometriosis.
Endometriosis is a condition characterized by heavy periods and debilitating pain during menstruation. Women are offered birth control to ease these uncomfortable symptoms, but again, it is only a band-aid covering up the root cause. While the research about this disease is minimal, what experts know at this point is that it appears to be autoimmune in nature. This means focusing on gut health and reducing inflammation are helpful to reduce symptoms naturally.
3: Fertility returns immediately after stopping
Many doctors assure women that they’ll have no problems conceiving after coming off the pill, but this false hope often results in heartbreak and confusion. On average, a woman can expect to wait 3-6 months post-pill before consistently ovulating again. – in rare cases, it can take as long as eighteen months.
4: It increases progesterone
Progesterone is a vital hormone that reduces anxiety, increases focus, and improves PMS symptoms. It is only produced after ovulation, which doesn’t occur on birth control. Instead, the pill contains a synthetic version known as progestin. Progestin does not offer the same benefits as progesterone, and in fact, is associated with an increased risk of depression.
5: You need to have a period while taking birth control
It is impossible to have a true period while on birth control. Instead, women experience what science calls a withdrawal bleed. This is a shedding of the uterine lining triggered by the cessation of hormone ingestion during the sugar pill week. However, it doesn’t offer any of the benefits of a natural period.
6: There are no symptoms associated with stopping the pill
Something called Post-Birth Control Syndrome is a myriad of unpleasant symptoms that can arise when a woman stops taking the pill. She might experience a return of previously suppressed symptoms or new issues that weren’t present, to begin with.
FINAL THOUGHTS ON THE TOP 6 MYTHS ABOUT BIRTH CONTROL
Millions of women take the birth control pill, but often for reasons other than its intention: preventing pregnancy. Doctors routinely prescribe the pill to suppress unpleasant symptoms such as acne and painful periods. However, it’s far from an ideal solution.
Doctors tell their patients that birth control regulates hormones, increases progesterone, and doesn’t cause any issues to arise after stopping. These are the top six myths about the pill. In reality, each is a band-aid that covers up the root cause of symptoms that can often be managed with lifestyle changes.