Your skin is the largest organ in your body. No wonder you feel so miserable when you get a rash or other type of inflammation. From chronic dry skin in the winter to oil problems in the summer, it’s not easy taking care of the genetic variations in your skin that you have.
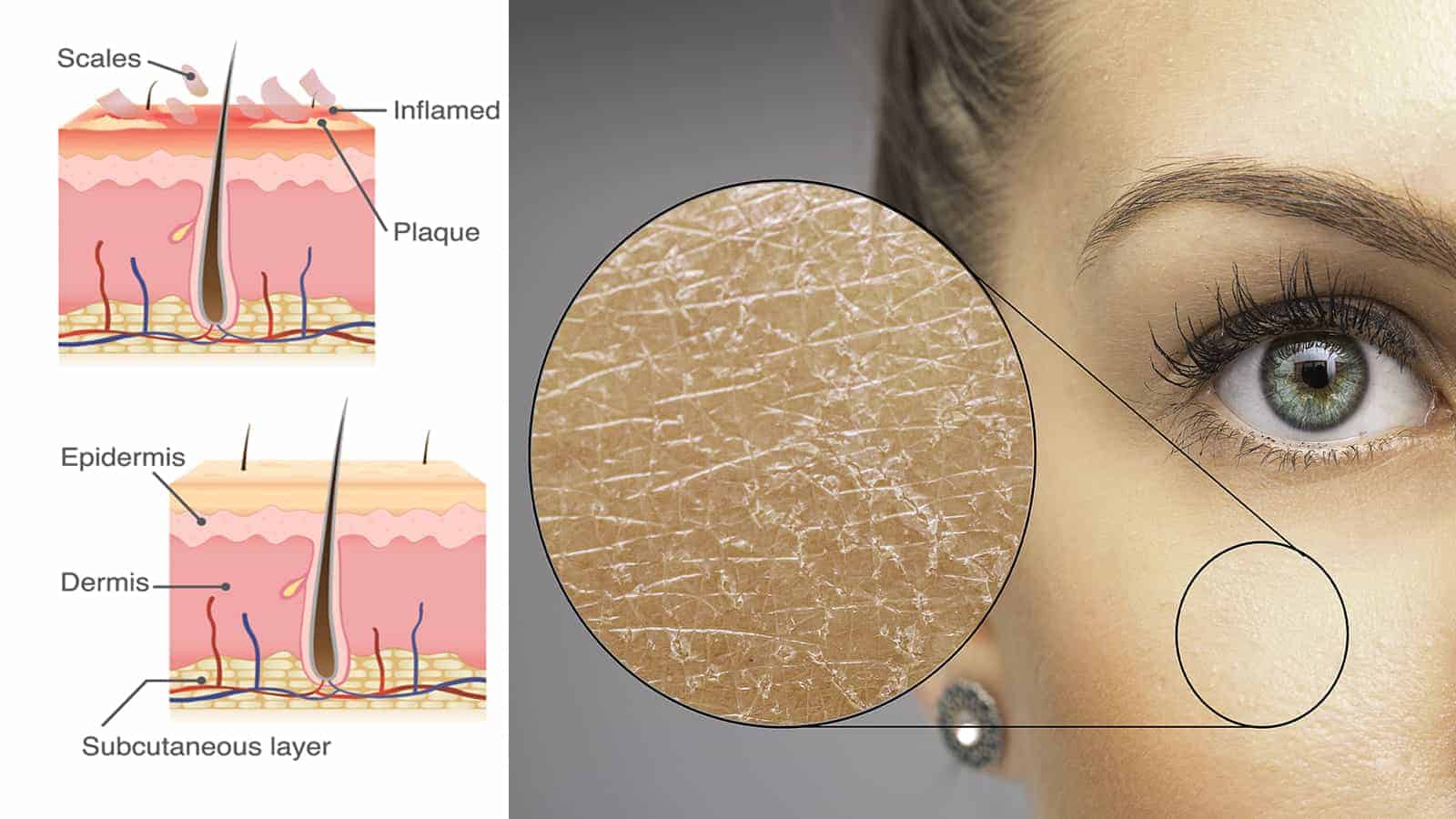
One of the most common skin irritations is atopic dermatitis, or as some call it eczema. It’s said to affect up to 12 percent of children and 10 percent of adults. It’s easy to identify this scaly condition as its trademarks are dry, thick, and itchy patches on the skin.
These patches are mainly observed in the folds of the skin. Many people confuse AD with psoriasis, which is another very itchy and dry condition. However, the two have some similarities but are quite different.
How Do You Know If You Have Atopic Dermatitis?
If you’re trying to distinguish AD from another skin condition, one of the things that doctors notate is the needling urge to scratch. It seems that you can’t leave your skin alone when these bumps and rash is present. Additionally, all the rubbing and scratching causes irritation.
It’s not uncommon for your skin to become inflamed and to weep and drain. Over time, the irritation will cause fluid-filled blisters to appear. These blisters can burst to leave an unsightly mess on your clothing. Scratching only makes things worse, but it seems that itching the area is unavoidable.
There is no need for medical tests to identify this skin condition as doctors know it when they see it. Though psoriasis and eczema are similar, they have some hallmarks that make them distinguishable. The first course of action is a topical cream to help ease the inflammation and urge to scratch.
Treating Atopic Dermatitis
Sadly, AD is a condition that is not curable, so it’s all about finding the treatment plan that works for you. You can quickly develop infections on the skin from scratching and introducing bacteria to open wounds. Secondary infections must be treated as they can become severe.
When creams aren’t sufficient, oral medications, including steroids, can be explored. Combination therapy is usually best. Studies have shown that stress can make AD worse, so flareups can become more common during times of angst and emotional upset.
How Does Genetics Variations Play a Part in Your Skin?
The medical community is continually studying AD and figuring out if and how they can resolve this nagging issue. Research conducted by the National Institute of Health reveals that they see some genetic links to this common condition.
When the skin lacks proper moisture, it’s easy to develop AD. The finding is astounding because identifying genetic variations could be the key to prevention.
Why Is the KIF3A Gene so Important?
It’s time for an in-depth science lesson. The reason why the KIF3A gene is so important is that it codes a protein that sends signals to the skin cells. This gene is what codes the skin to get the moisture it needs to thrive.
It isn’t very easy to understand the dealings of sensory mechanisms, but it’s a breakthrough finding. In previous studies, researchers found a link between KIF3A and children with asthma. They discovered that KIF3A and asthma run together.
Could genetic variations show susceptibility to this condition early so that parents could protect their infant from developing AD among other allergic disease mutations?
The gene KIF3A is responsible for creating a condition where water is lost from the skin; hence dry skin is the trademark of AD.
However, new research shows that some genetic variations in KIF3A were altered through methylation, which is where the gene is copied into an outline for protein production. It sounds extraordinarily complex, but it means that the KIF3A variants in those with asthma had higher rates of water loss in the skin than those without this breathing problem.
Can Low Levels of KIF3A Be Foretelling of AD?
Having lower levels of KIF3A was not substantial enough. Researchers needed to see if having these abnormal levels was the link to causing AD. They used mice to prove their theories, though none was harmed in the process.
When the mice had a dysfunctional skin barrier and increased water loss, they developed characteristics of AD. The conclusion was that genetic variations in the KIF3A protein caused dysfunction in the skin. So, the protein necessary to keep skin hydrated was missing, and thus AD developed.
These findings are astounding because they can now focus on intensive topical moisturizers that can restore hydration to the skin and prevent AD from developing. The prevention of AD could additionally prevent other allergic conditions in life.
Tests can be given to infants to show if they have these genetic variations of the KIF3A protein and are susceptible to AD. Then, rather than treating the aggravating symptoms associated with eczema later, they can manage the water loss issue to prevent it.
Since food allergies, asthma, and rhinitis also link to AD, it could be an astounding discovery to prevent all these painful conditions.
What About Adults Who Develop Eczema?
The study does little to help adults who suddenly develop AD later in life. Moving to a new climate or other forms of stress on the skin can cause this condition to develop. For instance, if someone lived in Florida where they were exposed to tropical climates and then move to Arizona, their skin can react to the changes in the atmosphere.
In Florida, the air is humid and warm. While the air is warm in Arizona too, it’s a very dry heat with little moisture. Those who have sensitive skin may find the move irritating and itchy.
Something as small as riding a plane from one side of the US to the other can induce symptoms. The changes in the atmosphere and the lack of moisture can affect the skin. When these conditions pop up later in life, the doctor may do a skin biopsy to ensure that you’re not dealing with another inflammatory issue.
Autoimmune conditions like lupus cause skin rashes and can be confused for something else before a definitive diagnosis is made. Additionally, a doctor will want to know both you and your family’s history when it comes to allergies. One hundred things can cause your skin to become inflamed, and AD shouldn’t always be the first to blame.
So, while the study was groundbreaking for helping to prevent AD from developing in children, these genetic variations do little to help adults with a sudden onset.
Astounding Statistics about AD
While ten percent of the adult population suffers from AD, did you know that it has a dramatic effect on their wallet too? Yes, the average person suffering from this skin condition will pay about $3,000 each year for treatment. Sadly, this is just the fees for seeing doctors and specialists to get help.
These numbers don’t include the costs of all the creams and other therapies. However, the math encompasses all measures to try to bring some sort of relief. Also, these folks are susceptible to a loss of productivity on their job. Did you know that people with AD often miss at least six days more each year than those who don’t have this condition?
When flareups reach their boiling point, doctors’ appointments, infections, and inflammatory conditions can leave people unable to work. Additionally, putting clothes on inflamed skin and wearing them for more than eight hours is unbearable.
Are Your Bad Habits Causing Your Eczema?
Did you know that your behaviors or bad habits can also affect your skin? Smokers are more likely to develop AD than those who don’t smoke. Everything points back to that hydration issue, and smokers have a loss of moisture in the body because of the toxins from cigarettes.
Furthermore, those who drink heavily can also have a problem. An abundance of alcohol in the system can be very damaging and can cause issues with hydration too. Sadly, the problems don’t stop there; adult AD is linked to higher odds of developing obesity, diabetes, high cholesterol, and hypertension. It can be a marker for heart disease too.
 Final Thoughts on Using Genetics Variations Research to Help Atopic Dermatitis Patients
Final Thoughts on Using Genetics Variations Research to Help Atopic Dermatitis Patients
While there is no cure for this condition, there are many effective management options to explore. It’s best to team up with a dermatologist from the cradle if these issues are present. While the studies regarding genetic variations are astounding, it’s too early in the game to put the data to use.
In the future, it may be possible to screen for abnormal variations of the KIF3A gene from birth. For now, it’s given hope that there may be early interventions in the future that can stop the suffering of children, and it may be the key to them having fewer allergy problems into adulthood.