Have you ever stood up too fast and felt so lightheaded you thought you might pass out? That is what a syncope (pronounced ‘sin-ko-pea’) episode feels like at its onset. Syncope is a more technical way of referring to the act of fainting. But it is much more complicated than you might think.
These fainting spells can happen for many different reasons. At the core of it is the fact that there is a sudden decrease in blood flow going into your brain. When this happens, you lose consciousness, and down you go to the floor.
Emergency room staff see syncope episodes every once in a while. It is estimated that about 3-5% of emergency room visits in the United States every year involve someone fainting. What’s more, about 42% of the population will experience a syncope episode at some point during their life.
So, why does this happen? Why is it happening to you? Is it something you should be concerned about? Let’s explore those questions as we take a further look into what causes fainting spells and what their symptoms can mean.
How Blood Flow Works
First and foremost, you need to understand how blood flow works throughout your body. Your brain and spinal cord both rely on two sources for blood: your vertebral arteries and internal carotid arteries, which branch off to form the middle and anterior cerebral arteries. This blood flow can change when you experience sudden bradycardia (when your heart beats at less than 60 beats per minute), a drop in blood pressure, or changes in blood flow to other parts of your body (like your legs).
Blood Flow and the Autonomic Nervous System
Syncope is a result of the interaction between the circulatory system and your body’s autonomic nervous system (ANS for short). Your ANS is responsible for maintaining your internal homeostasis. That’s just a fancy way of saying that it helps to regulate your blood pressure, body temperature, heart rate, fluids, and electrolytes. When these things are all in balance, you will likely feel alright and not have any fainting episodes.
If your ANS is unable to regulate your body’s systems, you’re going to have some problems. When you go to stand up, gravity will pool about 500 to 800 mL of blood in the distensible veins located below the heart. This pooling causes plasma volume to decrease by about 15% within 20 minutes of standing up. When your blood does not flow appropriately as a response, it pools in the veins. This situation triggers a reduction in your heart’s ability to pump blood, which then alerts your body’s compensatory mechanisms to act.
Those mechanisms include:
- the central autonomic network (CAN) mediating the sympathetic outflow upregulation
- skeletal muscles pumped in the legs
- the cerebral autoregulatory mechanism
- the renin-angiotensin-aldosterone system (RAAS)
The CAN, which is located in the brain stem, helps to coordinate the autonomic supply to your body’s cardiovascular system. There are pressure receptors that send impulses to the CAN when they detect a problem. That, in turn, triggers a flow of norepinephrine, which prompts your body to act. Your body thus experiences vasoconstriction, venoconstriction, and an increased heart rate. Constriction of veins will result in a correction of your orthostasis.
All it takes is 6 to 8 seconds of a stop in blood flow to the brain for someone to lose consciousness. That is how quickly your entire system responds to something as simple as a change in posture (e.g., going from sitting to standing).
Types of Syncope
There are several different types of syncope (and presyncope, which does not involve entirely passing out but does involve some loss of consciousness) that you should know about. Let’s take a look at each type individually and explain their different symptoms.
Reflex syncope
This type is the most common cause of fainting. As described above, your body’s reflexes stop working as they are supposed to. Your heart rate drops, as does your blood pressure. Hence, the blood flow to your brain ceases. In a matter of seconds, you pass out.
There are three sub-types here. These are:
- Vasovagal (This happens when your body overreacts to a stimulus, such as standing for too long or intense pain; this accounts for about 50% of reflex fainting cases.)
- Situational (This can happen when you do something like sneeze, cough, or laugh.)
- Carotid sinus (This can occur as a result of too much pressure placed on the carotid artery in the neck. Even things like wearing a choker necklace or moving your neck too quickly can cause this to happen.)
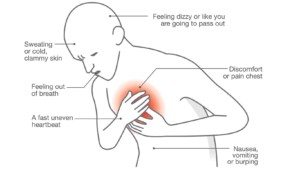
Symptoms most frequently associated with reflex fainting include:
- nausea
- feeling too warm
- tunnel vision
- feeling lightheaded
- visually blacking out
Cardiac fainting
This type of fainting is directly related to a problem with your heart. If you have structural issues like cardiomyopathy or a heart valve disorder, you could experience fainting. Electrical problems with the heart (such as arrhythmia) can also contribute, as can various other conditions, including a pulmonary embolism.
You are at risk for cardiac fainting if you are over 60 years of age, are male, have some form of heart disease, or have a known family history of cardiac conditions (especially if those family members have experienced fainting).
The most common symptoms of cardiac fainting are:
- passing out while you are lying down
- fainting or almost fainting while you are exercising your body
- feel heart palpitations or chest pain before passing out
Orthostatic fainting
As mentioned above, orthostasis involves how gravity impacts your blood flow when you change positions. Orthostatic fainting happens when you experience a blood pressure drop as you stand up. Your brain will try to stabilize this, but that doesn’t happen when you have orthostatic issues.
Causes for this condition can include:
- being dehydrated
- alcohol use
- recent blood loss
- taking certain medications (such as blood pressure or diabetes meds)
- having underlying health conditions (including multiple sclerosis and Parkinson’s)
Chiari malformation is another condition that involves fainting. Chiari is a type of structural defect of the skull that causes the cerebellum to compress on the brain stem, causing herniation. The condition Chiari involves intense cervical spinal pain. Since the CAN is located in this impacted area, ANS functions can become dysfunctional. Chiari patients present with a loss of balance and dysautonomia. Decompression surgery can help alleviate these symptoms.
With orthostatic fainting, you might notice warning signs that you are about to drop. Your vision might begin to tunnel or fade to black. However, this type of fainting can happen without any warning.
Cerebrovascular fainting
This type of fainting happens as a result of the blood vessels near and within the brain, not getting enough blood as that they can properly function.
Causes for cerebrovascular fainting can include:
- a cerebrovascular disease (such as an aneurysm or stroke) causing damage to the blood vessels
- Steal syndrome (which reverses the flow of blood to your arms from the subclavian arteries)
- basilar artery disease (a reduction of blood flow in the brain’s basilar arteries)
Those at risk for developing this condition are the elderly, those with cardiovascular disease, and those with cerebrovascular disease.
Symptoms of cerebrovascular fainting include:
- experiencing a headache
- feeling lightheaded or nauseous
- difficulty hearing
- confusion
- uncoordinated movements
Coping with Fainting
The best thing you can do if you feel faint is to lie down. Elevate your legs and keep your head low (in other words, avoid using a pillow for your neck and keep your entire spine as straight as possible). If you are not able to lay down on a firm surface, sit down. Putting your head between your knees can increase the blood flow to your brain. Stay in this position until your symptoms have passed and slowly get up. Do not rush it.
Afterward, you might feel just fine and not need any immediate medical attention. However, some folks will need to seek emergency medical help. Those people include the elderly, pregnant women, those with heart disease or diabetes, those who were injured in their fall, those who lost consciousness for more than a couple of minutes, those who lost control of bladder or bowel functions during their fainting episode, and those who have had these episodes happen on a somewhat frequent basis.
 Final Thoughts: Getting Diagnosed with Syncope or Fainting Spells
Final Thoughts: Getting Diagnosed with Syncope or Fainting Spells
It is crucial to speak with your doctor about the diagnosis. Doctors can diagnose your condition with tests like an electrocardiogram (ECG), a tilt-table test, a stress test, an echocardiogram, a CT scan, or an MRI. If you put off getting treated, your condition could worsen.
Do your best to avoid fainting spells. Stay hydrated, sit or lie down as needed, and don’t skip any meals. Pay attention to your triggers and seek medical attention if your situation becomes dire.