If you’re not sure of the difference between tendonitis and tendinitis, you’re not alone. Many Americans and, arguably, people around the world routinely mix up these two very different health problems. Of course, the fact that they have a similar spelling and sound nearly identical certainly doesn’t help matters.
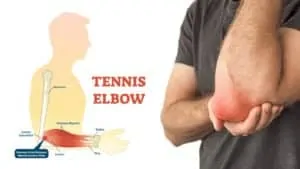
That said, the main difference between these two health conditions is that tendinitis is characterized by inflammation. Often this occurs following a sudden injury to a tendon. (Tendons are the tissue between the muscles and bones.)
Tendonitis, by comparison, does not cause inflammation and commonly links to a repetitive strain injury. Of course, there are many more differences between these two painful health conditions.
Everything You Need to Know About Tendinitis
Now we have a basic understanding of tendinitis, also commonly referred to as tendinitis-related tendinopathy. So let’s take an even closer look at what makes this condition different from tendonitis. First and foremost, tendinitis is most common in men and women over the age of 40.
Now you might be wondering. Why does age factor into this tendency? The condition stems from the fact that our bodies change with age. Indeed, the tendons in our body are no longer able to tolerate the same level of stress as they did when we were younger. As a result, they lose their elasticity and become increasingly susceptible to tearing, especially when performing repetitive tasks.
Undoubtedly, it is possible to develop tendinitis in any part of the body where tendons connect bones to muscles. However, the condition primarily impacts the following spots:
- Elbows
- Hips
- Knees
- Shoulders
- The base of the thumb
 The Achilles tendon
The Achilles tendon
Tendinitis-related tendinopathy can also affect the Achilles tendon, the largest tendon in the body. This particular tendon is a large and sturdy band of fibrous tissue. It connects the calf muscle to the calcaneus, also known as the heel bone. Not surprisingly, when an individual develops tendinitis of the Achilles tendon, they often have trouble running, walking, or even standing for long periods.
Who Is Most Likely to Develop Tendinitis?
Because tendinitis-related tendinopathy frequently results from repetitive strain injuries, it is not uncommon for it to impact individuals who engage in any of the following work-related activities:
- Sewing
- Typing
- Woodworking
- Shoveling
- Painting
- Gardening
Along with these work-related activities, playing certain sports, such as baseball, tennis, or golf, have also been shown to increase one’s chances of developing tendinitis-related tendinopathy.
Additional Risk Factors for Tendinitis-related Tendinopathy
Tendinitis-related tendinopathy, which, in addition to pain and inflammation, is characterized by damaged tendons with disorganized fibers, can also be caused by poor posture. Along with causing back pain, headaches, and even difficulty breathing, poor posture can place a tremendous strain on the group of muscles that make up the rotator cuff and the tendons of the bicep, all of which are needed to support the shoulder. When these muscles and tendons become inflamed, it is known as shoulder tendinitis.
That said, tendinitis-related tendinopathy of the shoulder can cause mobility problems as well as severe pain. Of course, repetitive strain injuries, age, and poor posture are not the only culprits when it comes to tendinitis-related tendinopathy as the condition can also stem from certain chronic diseases, including
Kidney disease
According to a study published by emedicinehealth.com, a consumer health information website, the probability of developing tendinitis-related tendinopathy increases exponentially for those diagnosed with chronic kidney disease, which is often the result of high blood pressure. Further, chronic kidney disease, which is also known as end-stage renal disease, can cause tendons in the quadriceps, triceps, and fingers to suddenly rupture, according to a separate study published by the National Institutes of Health. It is worth noting that certain blood diseases, such as leukemia, lymphoma, and myeloma, for example, can also cause these same problems.
Rheumatoid arthritis
Along with pain, stiffness, and inflammation, rheumatoid arthritis has also been linked to tendinitis-related tendinopathy. According to a question and answer segment published by the Arthritis Foundation, a nonprofit organization committed to supporting research into curing and possibly preventing arthritis, the same inflammation that causes joint damage in those with rheumatoid arthritis also damages connective tissue, including tendons and ligaments, in and around the joints.
 Everything You Need to Know About Tendonitis
Everything You Need to Know About Tendonitis
Having identified factors that can contribute to tendinitis-related tendinopathy and who is most at risk of developing the condition, let’s turn our attention to tendonitis. Also referred to as tendonitis-related tendinopathy, this condition is similar to tendinitis-related tendinopathy in that they can both trigger severe pain. And this has a lot to do with the micro-tears on the affected tendon. While tendonitis might not cause inflammation, the pain does become more intense with movement
Tendonitis-related tendinopathy arises from repetitive strain injuries. However, it usually results from a direct injury to the affected tendon, which can stem from a slip and fall, car accident, or any other kind of sudden blow to the body. Aside from the quicker onset of pain symptoms and the absence of inflammation, tendonitis-related tendinopathy is not too dissimilar from tendinitis-related tendinopathy. As such, the approach to treating or preventing either condition is nearly identical.
How to Prevent Tendonitis
Whether you have an occupation that requires repetitive movement, play sports, or have a chronic disease that causes inflammation of the tendons, there are things that you can do to minimize your chances of developing tendonitis or tendinitis-related tendinopathy. And it all comes down to taking a few steps to help keep your body and joints limber. That said, here are a few tips to help you get started:
Taking breaks
The human body has an uncanny way of letting you know when something is wrong. That said, if you’re experiencing pain while performing any activity, it would be a good idea to take a break. In doing so, you not only allow your body to recover but also any tendon that might be contributing to your pain symptoms.
Stretching
Along with keeping your muscles limber, stretching can go a long way toward fending off joint problems. Beyond that, it can help improve the range of motion in your joints.
Exercising
Performing weight-bearing exercises is yet another way to keep your joints, muscles, and tendons strong and healthy. Beyond that, doing so ensures that they can withstand the stress being put on them as you go about your day-to-day life. To get the most out of these exercises, consider doing some light stretching afterward.
Improving ergonomics
One of the most common forms of tendinitis-related tendinopathy among those who work in an office environment is carpal tunnel syndrome. And you can avoid it by improving your posture while sitting at your desk. Additionally, it is a good idea to make use of an ergonomic keyboard, chair, and desk whenever possible. According to a study published by Princeton University Health Services, well-designed ergonomic products can help take a lot of stress off of your tendons and joints.
 At-home Treatments for Tendonitis and Tendinitis
At-home Treatments for Tendonitis and Tendinitis
In most cases, you can relieve the sore feeling of tendinitis-related tendinopathy and tendonitis-related tendinopathy with a variety of at-home treatments.
- Acupuncture
- Resting the affected area
- Physical therapy
- Taking herbal supplements, such as turmeric
- Applying a cold compress or ice packs
When Should You Seek a Doctor’s Advice?
Generally speaking, you should start seeing relief from your symptoms within a few weeks after home treatment. Having said that, if your symptoms persist beyond this point or become worse, you should seek help from a physician.
If natural remedies do not resolve your issue
Some of the more common physician-prescribed treatments used to address tendinitis-related tendinopathy or tendonitis-related tendinopathy if your natural remedies do not provide relief might include:
Corticosteroid injections
This type of therapy can provide short-term relief from tendinitis-related tendinopathy and tendonitis-related tendinopathy. However, there is a caveat; overuse of corticosteroid injections can further weaken an already damaged tendon and increase the chances of it rupturing.
Phonophoresis
This approach to treatment involves using prescription-based topical anti-inflammatory creams, such as Voltaren, for example, and ultrasound to treat tendinitis-related tendinopathy or tendonitis-related tendinopathy. The sound waves from an ultrasound machine allow topical anti-inflammatory creams to deeply penetrate the skin and connective tissue, which helps relieve pain and inflammation that much faster.
Surgery
In severe cases, some physicians will recommend surgery to correct tendinitis-related tendinopathy or tendonitis-related tendinopathy, especially if either condition is causing mobility problems. A doctor might advise surgery if the affected tendon has already ruptured.
 Final Thoughts on Understanding Tendonitis Versus Tendinitis
Final Thoughts on Understanding Tendonitis Versus Tendinitis
All in all, tendinitis-related tendinopathy or tendonitis-related tendinopathy can both cause pain and mobility problems. Fortunately, there is a wide range of treatments available to those who are struggling with either condition.