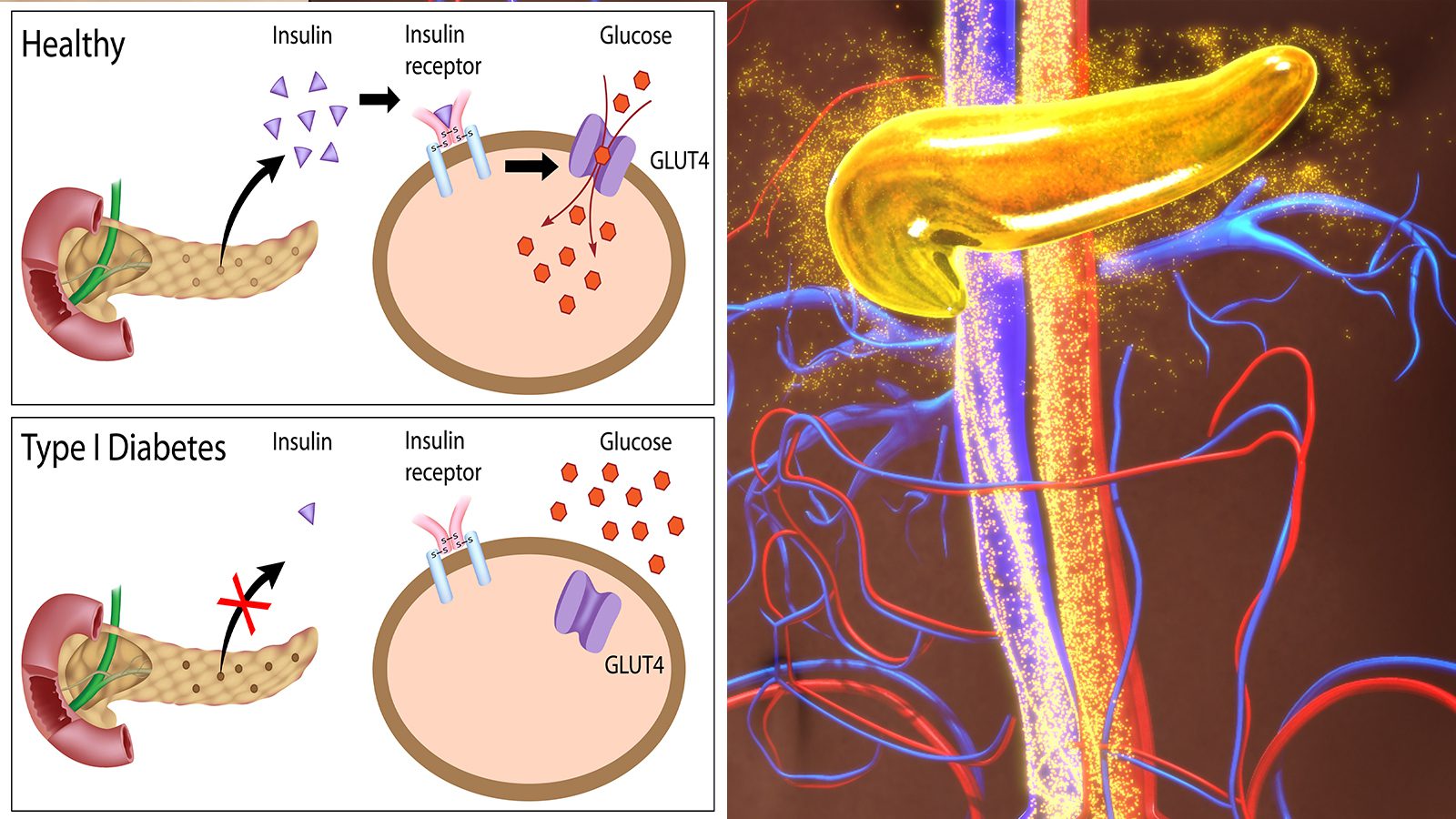
Researchers have discovered how nanotechnology could offer a new treatment for patients with Type 1 diabetes. Those with the condition must take insulin daily to manage blood sugar levels. Since it requires lifelong treatment, it’s burdensome for the patient.
Type 1 diabetes causes the immune system to attack and destroy insulin-producing cells in the pancreas. Therefore, patients must take the hormone either with an insulin pump or injection since their bodies can’t produce it naturally.
Current therapies, such as pancreatic islet transplantation, have been successful but have a few setbacks. It involves taking healthy islet cells from a deceased organ donor’s pancreas. Then, doctors inject them into a vein that transports blood to the liver of a person with type 1 diabetes. This procedure improves insulin production, so the patient no longer needs to take it; however, the immune system may reject new islets.
The patient may take immunosuppressive drugs during treatment, but they have unwanted side effects and insufficient protection for transplantation cells. Therefore, the current treatment options might not work long-term.
Meet the Research Team from Northwestern University
However, a team of researchers from Northwestern University believes they have discovered a breakthrough treatment. The technique utilizes nanocarriers to reformulate the widely used immunosuppressant rapamycin. Using these nanocarriers, the team created a new type of immunosuppression that can target specific transplantation cells. This way, other immune responses aren’t affected.
The paper, published in Nature Technology, may lead to revolutionary treatments for type 1 diabetes. Evan Scott, the Kay Davis Professor and an associate professor of biomedical engineering at Northwestern’s McCormick School of Engineering, led the Northwestern team. Another contributor was Guillermo Ameer, the Daniel Hale Williams Professor of Biomedical Engineering at McCormick and Surgery at Feinberg.
Jacqueline Burke was the first author of the study. She’s a National Science Foundation Graduate Research Fellow and researcher working with Scott and Ameer at the Center for Advanced Regenerative Engineering (CARE).
Researchers Discover Breakthrough Treatment for Type 1 Diabetes
Ameer’s research focused on improving islet transplantation by engineering the islets’ environment. To do this, he used biomaterials to enhance their survival and function. However, this method still didn’t address the problems resulting from traditional immunosuppression therapies.
“This was an opportunity to partner with Evan Scott, a leader in immunoengineering, and engage in a convergence research collaboration that was well executed with tremendous attention to detail by Jacqueline Burke, a National Science Foundation Graduate Research Fellow,” Ameer said.
Rapamycin, a well-known immunosuppressant drug, impacts many cell types throughout the body. Patients usually take this orally. However, patients must pay close attention to dosage, as too much can cause harmful side effects. Moreover, lower doses aren’t as effective in islet transplantation cases.
Scott wanted to enhance the drug by placing it in a nanoparticle to control its movement to overcome these shortcomings effectively.
What the Researchers Said
“To avoid the broad effects of rapamycin during treatment, the drug is typically given at low dosages and via specific routes of administration, mainly orally,” Scott said. “But in the case of a transplant, you have to give enough rapamycin to systemically suppress T cells, which can have significant side effects like hair loss, mouth sores, and an overall weakened immune system.”
After a transplant, immune cells, or T cells, reject the unfamiliar cells and tissues. Immunosuppressants can prevent this side effect and affect the immune system’s overall functioning. However, the team’s engineered nanocarrier and drug combination would target specific cells to avoid impairing the immune system. The nanoparticle would pinpoint and modify antigen-presenting cells (APCs) for more controlled immunosuppression.
Using nanoparticles also had another advantage. It allowed the team to deliver rapamycin through a subcutaneous injection using a metabolic pathway different from standard oral administration. It avoided excess drug loss in the liver by reducing the dose necessary for effectiveness – about half the usual dose.
“We wondered, can rapamycin be re-engineered to avoid non-specific suppression of T cells and instead stimulate a tolerogenic pathway by delivering the drug to different types of immune cells?” Scott said. “By changing the cell types that are targeted, we actually changed the way that immunosuppression was achieved.”
How Immunoengineering Could Impact Type 1 Diabetes
For the study, the team introduced diabetes to mice subjects before treating them. They gave them a combination of islet transplantation and rapamycin, delivered orally and via nanocarrier. The day before transplantation, the team gave the mice injections of the modified drug and continued the regimen every three days for two weeks.
Luckily, the team didn’t notice many side effects in the mice and found no trace of type 1 diabetes throughout the 100-day trial. However, the treatment should last a lifetime. Also, the team discovered that the mice treated with the nano-delivered drug had a more robust immune response than mice given standard treatments.
Scott said enhancing and controlling a drug’s side effects via nanotechnology isn’t revolutionary.
“But here we’re not enhancing an effect. We are changing it — by repurposing the biochemical pathway of a drug, in this case, mTOR inhibition by rapamycin, we are generating a different cellular response.”
The team’s findings could also lead to improved treatments for other conditions.
“This approach can be applied to other transplanted tissues and organs, opening up new research areas and options for patients,” Ameer said. “We are now working on taking these very exciting results one step closer to clinical use.”
Burke was also incredulous after seeing the study’s results. When she saw the mice’s blood sugar drop dramatically, she kept double-checking the readings to ensure their accuracy. However, the number remained stable throughout the study period.
The Northwestern team made a breakthrough indeed in type 1 diabetes. They’ve been studying islet transplantation for three years and say the latest findings could significantly impact diabetes research.
Scott has started working on patenting the treatment for diabetes and collaborating with leaders in the industry. The next phase of research will involve clinical trials. When the cure becomes commercially available, it will eliminate the issues involved with current technologies like pancreatic islet transplantation.
Final Thoughts on New Treatment for Type 1 Diabetes
The latest research by Northwestern University could have important implications for those with type 1 diabetes. The team discovered a way to target specific pancreatic cells to deliver an immunosuppressant drug. Using nanocarriers, they re-engineered the common immunosuppressant rapamycin to generate a different cellular response. Hopefully, the treatment will soon become commercially available for type 1 diabetes.